The Institute of Pennsylvania Hospital, Philadelphia, Pennsylvania 1939, and University of Pennsylvania, Philadelphia, Pennsylvania 19101
Few phenomena are as impressive as the use of hypnosis to induce surgical anesthesia. Simply by listening to the hypnotist, the patient appears to go to sleep, and, in response, to appropriate suggestions, appears to become insensitive to pain, allowing major surgery to be carried out. Its use as an anesthetic was first reported in 1829 during a breast amputation by Cloquet, a French surgeon. Though there were isolated instances of mesmerism, as it was then called, employed as surgical anesthesia on the continent and in England, there was considerable opposition to its use. A young surgeon, Esdaile (6), in charge of a public hospital in India, however, used hypnoanesthesia with several hundred patients, publishing a report of his results in 1850. It is curious that violent objections should have been raised to this safe and, at least occasionally, very effective procedure at a time when chemical anesthesia was not yet available.
In recent times, the fact that it is possible for a suitable patient to remain comfortable with hypnosis as the sole anesthetic during major surgery has been well documented in procedures ranging from appendectomies to thyroidectomies, from cesarean sections to cardiac surgery (for a review, see ref. 12). It is understandable that with the ready availability of essentially safe chemical anesthesia, the use of hypnosis as a surgical anesthetic finds limited application. Nonetheless, hypnotically induced anesthesia dramatically demonstrates the ability of psychological procedures to suppress a patient's appreciation of pain. Therefore, just as it is difficult to understand why mesmeric anesthesia was not employed prior to the availability of chemical anesthesia, we now may wonder why psychological techniques are not more widely employed in dealing with chronic pain where chemical control is by no means fully satisfactory. I suspect the major reason for this hesitancy -- in the 19th century as well as today -- is related to the ingrained belief that when pain is caused by physical stimuli, the only effective way that it can be controlled is to somehow alter the neural mechanisms by which pain is transmitted or perceived.
In order to meaningfully discuss the mechanisms of psychological control of pain in general and hypnotic control of pain in particular, it is important to first consider the nature of pain itself, and secondly, to consider the nature of the hypnotic phenomenon.
155
156 HYPNOTIC CONTROL OF PAIN
THE NATURE OF PAIN
Even by restricting the discussion to pain primarily due to pathologic processes in body tissue and omitting any consideration of pain due to psychologic or operant mechanisms, there would still be considerable controversy about a fully satisfactory definition of pain. Generally, one considers the pain-inducing stimulus and the pain response, behaviorally, physiologically, and in terms of the patient's report about his experience. By grouping all of these together one may well think of pain as an objective phenomenon (which may be reified further as a set of neural impulses in the spinothalamic tracts, in the thalamus, or limbic system).
If, however, we ask which of these aspects of pain really indexes the phenomenon, the answer is by no means straightforward. Certainly the application of a pain-inducing stimulus is not sufficient to define pain, since the afferent impulses can be modulated or even interrupted at a variety of levels. Again, behavioral correlates of pain, such as grimacing, convulsive movements, moaning, and similar pain behavior do not define it. Stoics are capable of suppressing such behaviors, frightened individuals may manifest them in anticipation of a pain stimulus, and an actor may produce them at will. Even physiological correlates of pain, such as increased skin conductance, respiratory changes, and transient slowing of the heart rate, are not accurate indices since they are produced by a variety of stimuli other than pain, and, further, the magnitude of autonomic responses is often modulated as much by the level of anxiety as the pain sensation as such.
Thanks to pharmacology, it is possible to observe a dissociation of the various correlates which, under normal circumstances, covary with pain. When a patient is put to sleep with thiopental and exposed to painful stimuli, he may well grimace, writhe, and, in addition to the behavioral changes, may also show the physiological correlates of pain. Nonetheless, as long as the patient is asleep and has no memory of a painful sensation on awakening, it seems inappropriate to speak of his having had pain. Further, when giving thiopental combined with succinylcholine anesthesia, the former prevents the appreciation of pain while the latter effectively prevents all behavioral evidence of pain, since it induces a total paralysis of all voluntary muscles. As a consequence, the patient not only is without pain but also does not show any behavioral consequences in response to the pain stimuli.
That these are totally different functions, however, is a fact that is made all too clear by the occasional unfortunate instances when patients had been awakened because they had been given insufficient amounts of thiopental or other general anesthetic but were unable to indicate that they were awake because they were totally paralyzed with a muscle relaxant. Under these circumstances, surgery continues with the patient showing no external evidence of pain though experiencing great agony. It is easy to comprehend how this could happen since behavioral evidence of pain would normally alert the anesthesiologist to
157 HYPNOTIC CONTROL OF PAIN
the need to administer more drug. So ingrained is the link we make between behavioral signs of pain and pain that one tends not to consider the possibility that a relaxed patient could be hurting even as he is being respirated, since the curare-like action of the drug has paralyzed all muscles.
As a consequence of dramatic malpractice suits, this particular mistake is unlikely to occur today. Nonetheless, it demonstrates the power of the almost universal assumption that severe pain is always associated with the overt behavioral signs of experiencing pain. In the final analysis, the one component of pain that is crucial is the experience of hurting. Sternbach (24) aptly characterizes pain as "a personal, private sensation of hurt" (p. 12). In the absence of that sensation, it makes little sense to speak of pain regardless of the outward appearances and physiological responses of the patient.
Yet it is, of course, never possible for one individual to really know what another is experiencing. Thus, we infer the presence or absence of pain from what we know about the stimulus as well as the patient's behavior, his physiological responses, and his reports about his experience. There is an interesting paradox in the weight given to the patient's verbal description. Clinically, if we have reason to trust the patient as a reliable reporter of his subjective experience, his verbal statements become the single most important source of information about his pain. On the other hand, there may be reason to suspect the verbal report, either because the patient is felt to be unreliable or because the report is contradicted by behavioral or physiological evidence as the better index of the patient's experience.
It is beyond the scope of this chapter to consider in detail the circumstances which affect how we judge the pain of others; it is important, however, to remember that neither behavioral nor physiological responses are pain; they are useful only as correlates which help us to assess the "private, personal experience of hurt" in others.1
RELEVANT ASPECTS OF HYPNOSIS
Like pain, hypnosis has no single satisfactory definition. It is useful to distinguish between a hypnotic-induction procedure on the one hand, and the extent of the hypnotic response of the patient on the other. Further, it is useful to recognise that there is no item of behavior carried out by the hypnotized subject that he would not carry out if simply asked to do so in the waking state. 2
To illustrate a typical hypnosis experiment, a responsive subject is asked to
2 It must be kept in mind that hypnosis is never induced in a vacuum but occurs only in three types of contexts: (a) experimental, (b) therapeutic, and (c) a demonstration. Each of these contexts involves a tremendous degree of behavioral control, and for this reason no increment of control over behavior has as yet been demonstrated following the induction of hypnosis. (For a discussion of these issues, see ref 19.)
158 HYPNOTIC CONTROL OF PAIN
relax and focus his mind on some particular point, and as one suggests relaxation, his eyes become heavy and they begin to close. As one continues to make suggestions, the subject becomes progressively able to respond to these suggestions. If told the fingers of his hand are light as a balloon and that the hand will float upward, the hand will seem to slowly lift upward into the air. If he is told the room is cold, he will show signs of becoming uncomfortably cold and may begin to shiver. If it is suggested that there is a fly in the room and it is annoying him, he will try to shoo it away. If it is suggested that he is unable to see a box that is in front of him, he will insist that there is nothing there. Finally, if before awakening, the subject is told to forget all that has occurred, he will have little or no recall, perhaps describing his experiences as if he had been asleep.
A demonstration of this kind strikes the observer as compelling, perhaps even incredible. Consider, however, the reason for such a response. It is not, the fact that the subject raises his hand. After all, simply asking a patient to raise his hand will elicit universal compliance. Rather, it is that the patient's hand seems to rise upward slowly as if he were experiencing the sensation of floating. Indeed, if we had asked him about the experience at the time he would almost certainly have described it as such, and if we ask him to remember what occurred, he will report his hand felt light and it seemed to rise by itself without any effort. Similarly, when the subject was told that there was a fly in the room, it is not that he moved his hand about that strikes the observer, rather that this movement appeared to reflect the experience of being bothered by a fly. If we analyze each suggestion, the patient's response is characterized as indicating hypnosis because it involves a distortion of either perception or memory, and the behavior itself tends to be experienced as nonvolitional. When these characteristics are present, we may diagnose the individual as being hypnotized.
Another very important attribute of hypnosis is that there are wide differences in the way individuals respond. The identical induction procedure will cause some subjects to be profoundly responsive to virtually all hypnotic suggestions; others will not be affected at all, with the bulk of the population showing various degrees of response. Since the hypnotic induction procedure induces hypnosis only in some individuals, merely knowing that a patient has been exposed to an induction cannot tell us whether he is hypnotized. Furthermore, some highly responsive subjects may enter hypnosis even without any formal induction, To the degree that they are capable of experiencing suggested changes in parception or memory, and feel themselves acting without volition, they must nonetheless be considered as hypnotized. In other words, some individuals do not need formal induction procedures to manifest hypnosis, while others will fail to manifest hypnosis despite induction procedures.
Some hypnotic suggestions are difficult to respond to and require a greater hypnotic skill on the part of the subject than others. For example, depending upon how one scores success, some two-thirds of unselected volunteers will
159 HYPNOTIC CONTROL OF PAIN
give evidence of hand levitation, whereas only 35% of such a normal population is able to experience a fly, and even of these only some experience the hallucination as totally convincing (11, p. 216). Again, only 9% respond to a negative visual hallucination (p. 238). On the other hand, some 30% show some degree of amnesia in response to suggestion (pp. 216, 238).
Since different hypnotic items vary in their difficulty, a series of such items can be used to assess the degree of hypnotic responsivity of any given individual (22,25,26). One important fact has emerged from a large number of studies of this kind: The skill of entering hypnosis depends on the ability of the subject, with the ability of the hypnotist having little or no effect. Further, the skill of entering hypnosis is a remarkably stable trait of the individual which persists over years.
Given the dramatic changes that hypnosis can bring about, it is hardly surprising that many observers assume that there are profound neurophysiological alterations associated with hypnosis. Nonetheless, despite extensive research, no physiological changes unique to hypnosis have been identified (e.g., 21), nor is it even necessary for the hypnotized individual to be relaxed. Banyai and Hilgard (2) have shown, for example, that responsive subjects could readily be hypnotized while working on an exercycle without interrupting their physical activity.
In sum, then, hypnosis is a phenomenon that is characterized by the ability of the subject to respond to suggestions with appropriate alterations of his perception or memory and with the feeling that his behavior occurs as if by itself, without volitional effort. Though usually brought about by an induction procedure involving suggestions of relaxation, neither the induction procedure nor relaxation is essential. The single most important determinant of the subject's response appears to be a kind of ability that varies with the individual and is a relatively stable attribute. Finally, the essence of the hypnotic phenomenon, like the essence of pain, is to be found in the subject's experience.
THE EFFECTS OF HYPNOSIS ON PAIN
Let us again consider hypnotic anesthesia for surgery. What is it that impresses the observer? Certainly, to carry out major surgery on a fully conscious individual without any pain is not a difficult matter. Local anesthesia, while tedious, presents limited difficulty, and spinal anesthesia is widely employed. The big difference is that the hypnotic intervention seems so trival and somehow unlikely to be capable of suppressing pain. Furthermore, hypnotic anesthesia, like pentothal, does not tend to totally suppress the behavioral signs of pain, nor the physiological reflex reactions to pain. The increase in skin conductance, the changes in respiration, the increase in blood pressure, and the effects on heart rate can all be seen even in the deeply hypnotized subject who firmly asserts he feels no pain. The presence of the behavioral and physiological correlates of pain, combined with the absence of what would seem to be an adequate procedure
160 HYPNOTIC CONTROL OF PAIN
to prevent pain, has led some observers to question whether hypnotic analgesia even exists.
Esdaile (6), writing in 1850, already encountered this form of skepticism. A commission sent to examine his work filed an equivocal and unflattering report about seeing 6 patients operated on for tumors of varying sizes, all of whom denied any discomfort, 3 of whom seemed relaxed and comfortable, but the other 3 showed behavioral signs of discomfort. Though it is noteworthy that in the absence of any anesthesia, all 6 patients reported being comfortable throughout the procedure and did not require being restrained, it was still argued that all of these patients were simply being stoical and must have experienced the pain. Esdaile's comments about his practice to those who doubted the patients' veracity are worthy quoting:
Since then [referring to the introduction of hypoanalgesia] I have had every month more operations of this kind then take place in the native hospital in Calcutta in a year, and more than I had for the six previous. There must be some reason for this, and I only see two ways of accounting for it: my patients, on returning home, either say to their friends similarly afflicted, "Wah! brother, what a soft man the doctor Sahib is! He cut me to pieces for twenty minutes, and I made him believe that I did not feel it. Isn't it a capital joke? Do go and play him the same trick; you have only to laugh in your elbow, and you will not feel the pain." or they say to their brother sufferers, "Look at me; I have got rid of my burthen [of 20, 30, 40, 50, 60, or 80 lbs., as it may be,] and am restored to the use of my body, and can again work for my bread: this, I assure you, the doctor Sahib did when I was asleep, and I knew nothing about it; -- you will be equally lucky, I dare say; and I advise you to go and try; you need not be cut if you feel it." Which of these hypotheses best explains the facts my readers will decide for themselves... (p. 219)
In more modern terms, there is much behavioral data which supports the patient's insistence that he is comfortable during hypnotic anesthesia. Thus, women who have once delivered a child painlessly under hypnosis typically prefer this procedure for subsequent deliveries. Patients not only maintain that they feel no pain in talking to the physician or the nurse but also give similar reports to friends and family. Subjects who participated in our studies involving pain often expressed a willingness to take part in future work as long as it did not involve pain stimuli for which there was no hypnotic analgesia.
Nonetheless, attempts to explain away hypnotic analgesia persist to this day. Barber, 3 for example, in discussing a caesarean section with hypnosis as the sole anesthetic, sought to argue that the procedure itself simply was not very painful: Once the skin incision was completed the muscle tissue does not tend to have many pain receptors, and the peritoneum, while sensitive to stretching, was not as sensitive to being cut, and so on. While this explanation did not gain many converts among medical members of the audience, the fact that it
161 HYPNOTIC CONTROL OF PAIN
was proposed at all by a serious scientist in the 1970s and accepted as a viable explanation by some members of the audience, speaks to the difficulty of accepting the patient's assertion that she was comfortable despite the presence of pain stimuli.
There are, however, difficult and complex issues involved in the hypnotic suppression of pain. In series of systematic studies, Hilgard and Hilgard (12) showed that highly hynotizable subjects, who are able to tolerate intensely painful stimuli with few behavioral signs of pain while reporting little or no discomfort, nonetheless at another level perceive pain. Thus, when asked to rate pain by means of automatic writing or simply by addressing that part of the individual that is not normally conscious, they give substantial pain ratings; lower than ratings evoked by similar stimuli without hypnosis but very substantially more than they otherwise report during hypnosis or, if asked to recall their experiences, after hypnosis. The implications of these fascinating observations speak to the presence of dissociation phenomena that may have much to do with the mechanisms of hypnotic pain suppression. They do not, however, alter the hypnotized patient's conviction that he is comfortable during the procedure or his memory subsequently that he had been comfortable while the procedure was going on.
The Effect of Individual Differences in Hypnotizability on Hypnotic Pain Suppression
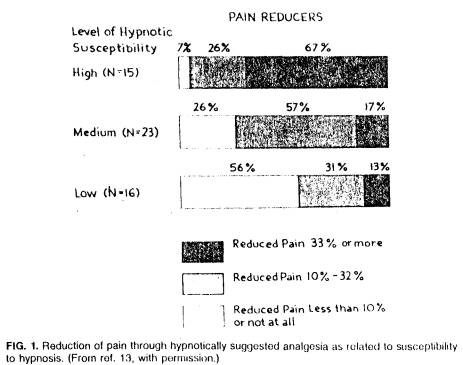
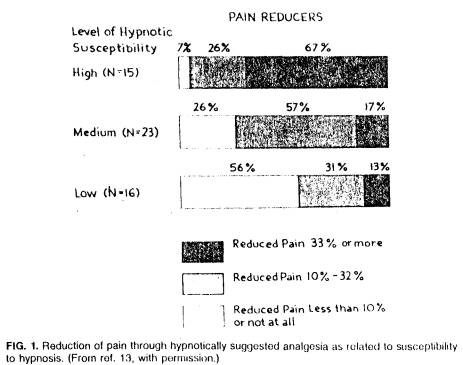
Recognizing that individuals differ in their ability to respond to hypnosis, it should follow that those more able to respond should derive more benefit from hypnotically suggested analgesia. Hilgard and Morgan (13) compared the responses of three groups of subjects -- of high, average and low hypnotizability -- to suggestions of hypnotic analgesia during a cold pressor test. Using subjects' pain ratings as a criterion measure, they showed that of 15 highly hypnotizable subjects only 7% failed to reduce pain less than 10%, while 67% reduced pain by 33% or more. Conversely, with 16 subjects who had little ability to enter hypnosis, 56% showed less than 10% pain reduction and only 13% reduced pain by 33% or more (see Fig. 1). As you will note, the group with middle hypnotic responsivity falls between these two groups.
Clearly, the ability of the subject to benefit from hypnotic suggestion in a laboratory setting is closely related to his ability to respond to other kinds of hypnotic suggestions. The question arises whether or not the same is true in clinical settings. Few studies have directly addressed this issue. Fortunately, Gottfredson (10), in an elegant dissertation, was able to assess hypnotizability of patient volunteers prior to undergoing dental treatment. Of the 29, patients asked, 25 volunteered and agreed to having at least one of their regular dental sessions with hypnosis as the only anesthesia. For comparison, at least one other session utilized a local anesthetic. The order of the sessions was randomized and did not affect the findings. All subjects were tested with a standard laboratory test of hypnotic responsivity (Stanford Hypnotic Susceptibility Scale, Form A,
162 HYPNOTIC CONTROL OF PAIN
[25]). Subjects had the option of requesting chemical anesthesia at any time. Four subjects availed themselves of this option within one minute of beginning the procedure and prior to any pain ratings. These will be excluded from consideration here. Of the remaining subjects, all 9 highly hypnotizable individuals completed the treatment under hypnosis without any chemical supplement, whereas only 5 of the 12 mediums and lows completed the treatment without any supplement. The amount of pain correlated with hypnotizability -.56, df = 19, p < .005.4 The ability of the subject to respond to hypnosis is a major factor in the degree of relief that is obtained in the clinical dental context or in the laboratory. 5
Similar findings which speak to the importance of the patient's ability to respond to hypnosis in order to obtain pain relief are summarized by Hilgard and Hilgard (12). Generally, there is a clear association between hypnotizability
5 This study was not carried out blind and the possibility of inadvertent bias affecting the results cannot be excluded. Further, in a later study, Joseph Barber (3), using a smaller sample and different procedures, failed to show a relationship between hypnotizability and degree of pain relief in a dental context. However, these observations may well be due to procedural differences, and in pilot work with our laboratory, hypnotizability as an attribute of the subject again appeared to be the major determinant of the subject's response, even with Dr. Joseph Barber conducting the rapid hypnotic procedures he had used in his 1977 study.
163 HYPNOTIC CONTROL OF PAIN
and the extent of relief from pain. While this will vary with circumstances, it may approximate .6 as in the Gottfredson study, but it is never perfect: Thus there are always a few individuals with relatively low hypnotic responsivity who nontheless derive considerable benefit. We shall return to this point later in our discussion.
Hypnotizability, the Placebo Response, and Pain Relief Through Suggestion
One tends to think of the placebo response as a manifestation of the same psychological processes which account for hypnosis. Elsewhere (17,18) we have reported in-depth findings that challenge such an assumption. We will outline the relevant aspects of this rather complex study here because it speaks to some basic questions about the nature of hypnotic analgesia.
The response to suggestions of anesthesia following an induction procedure was compared between two groups of subjects, 12 highly hypnotizable individuals and 12 subjects who had repeatedly failed to respond to hypnosis. One of the problems with such a comparison, however, is that the latter unhypnotizable group will not only fail to enter hypnosis, but also do not expect hypnosis to be of help to them, whereas those individuals able to enter deep hypnosis have every reason to believe that this technique should help them tolerate pain. Since our interest was to compare the effect of hypnosis, we wanted both groups to have the expectation that this method would be of help to them. For this reason, the unhypnotizable subjects participated in yet another hypnotic induction session with a different investigator, which was carefully designed to utilize elaborate relaxation procedures over a long period without, however, any hypnotic suggestions being given, since these subjects would almost certainly have failed to respond to any of these.
After a procedure lasting some 50 min which induced profound relaxation, a phenomenon that is quite unrelated to hypnosis, another lengthy technique was used to induce glove anesthesia of the right hand. Without asking the subject to comment on the anesthesia, he was asked to tolerate a mild shock, which was administered to both his right and his left hands. The subject was subsequently awakened with instructions to have lost track of time but otherwise to recall everything that had happened. (Again, even unhypnotized individuals become unaware of the passage of time during a lengthy procedure of this kind.)
When asked, all of the subjects indicated that, much to their surprise, this time the hypnotic procedure had been elective and that there was indeed a modest but striking difference in the electric shock between the right and left hand. They typically expressed considerable satisfaction that they had finally been able to achieve a hypnotic experience and eagerly looked forward to participating in further studies. The manner in which this result was achieved, however, had little to do with hypnosis. When the experimenter tested the right hand, he simply decreased the amount of current applied to the hand without, of
164 HPNOTIC CONTROL OF PAIN
course, informing the subject. The manner in which the testing was presented to the subject was as though the experimenter merely wanted to assess his response, and the investigator indicated that he too was pleased that the subject had been able to have the experience. Carefully carried out, the manipulation was extremely plausible and resulted in a group of subjects still unable to respond to hypnosis but sharing the conviction of the hypnotized group that they would benefit from hypnosis when attempting to control pain.
All subjects subsequently came to the laboratory and participated in an ischemic pain procedure, which involved applying a blood pressure cuff at 200 mm Hg to their arm and then asking that they pump water by means of a rubber bulb from one flask to another. This task becomes exceedingly painful as the amount of ischemia mounts. Subjects were asked to indicate pain threshold but to then also continue pumping as long as possible. Both the time blood flow is occluded and the amount of work performed have been shown by others (5,15) to be systematically related to pain threshold.
The experimenter was kept blind concerning the subject's ability to enter hypnosis. After an initial base-line session, subjects were asked to return for a second session which would involve hypnosis. During that session, hypnosis was induced by the same relaxation procedure mentioned earlier, and the experimenter was also careful to avoid any test of hypnotic responsivity which would indicate whether the subject was, in fact, hypnotizable. He then suggested analgesia of the hand and arm and repeated the same test. Again, pain threshold and tolerance were assessed.
Finally, the subjects were asked to come again for yet a third session during which it was explained to them that a powerful analgesic would he employed to assess how long and how much water they could pump if the pain were effectively controlled and the only limiting factor were the amount of anaerobic energy in the muscle. Subjects were given a pill, and about 20 min later the ischemic muscle test was again repeated. (Though all subjects received placebo, all members of the laboratory -- other than the director -- believed that a double-blind comparison was being carried out between Darvon ® and a placebo. Thus, the placebo was given with conviction by the investigator, while we had the benefit of having all subjects in the placebo treatment.)
Figure 2 summarizes the basic findings for pain thresholds and pain tolerance across all three sessions. Note first that the level of response to placebo in session 3 was virtually the same for the highly hypnotizable group as for the unhypnotizable group. There is no meaningful difference in the level of placebo response found between these two groups. Certainly this speaks against the notion that hypnotizability is related to the placebo response.
Looking at the placebo response of the unhypnotizable group, it is interesting that the magnitude of response overall is virtually the same as that to hypnosis. Indeed, there is a correlation of .76 between the amount of pain relief the unhypnotizable subject obtains from hypnosis and placebo. However, if one examines the hypnotizable group, it is obvious that the amount of benefit they
165 HYPNOTIC CONTROL OF PAIN
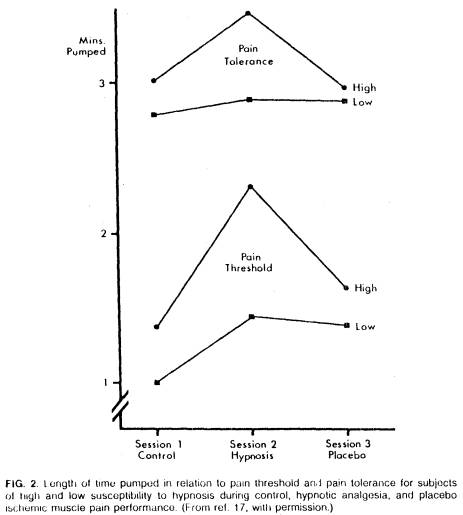
derive from hypnosis is vastly greater than the amount of benefit they derive from placebo. Of course, it would be possible for hypnosis to be more effective but, nonetheless, a high correlation could exist between the response to hypnosis and placebo in highly hypnotizable subjects. Again, this is not the case. On the contrary, within this group the relationship of pain relief from hypnosis and pain relief from placebo is .06.
Examining Fig. 2, it is clear that the hypnotizable group derived significantly more benefit from hypnosis than the unhypnotizable group, but their response to placebo is no different from the unhypnotizable group. The dramatic effect of hypnosis on pain cannot be explained in terms of subject's expectations, but rather, again, turns out to be directly related to hypnotizability. Nonetheless,
166 HYPNOTIC CONTROL OF PAIN
the unhypnotizable subject also derives considerable benefit from hypnosis. While less than the amount of benefit seen in the hypnotizable individual, the effect is still significant. Since this effect is highly correlated with the amount of relief obtained by placebo, we have conceptualized it as a placebo effect of the hypnotic procedure. While for some purposes it is useful to think of it in this fashion, in the context of the present discussion it points up important effects on the hypnotic-induction procedure which occurs even if the subject fails to be hypnotized. It appears to us that these effects are worth studying in their own right and may, in many instances, be extremely important clinically.
Effects of the Hypnotic Induction Procedure on Unhypnotizable Individuals
The hypnotic induction procedure is usually assessed in terms of its effectiveness in inducing hypnosis in a subject. As I have tried to stress throughout this chapter, whether the patient enters hypnosis is primarily a function of his ability to do so. Motivational factors may readily impede his ability to enter hypnosis, but for the most part, if subjects are moderately cooperative, are not negativistic, and have a moderately good relationship with the operator, motivation does not appear to be particularly important. Rather, the response then depends upon the individual's skill of entering hypnosis.
Nonetheless, the induction procedure is not without effects, even for those individuals who are unable to experience hypnosis. In an interesting series of studies, London and Fuhrer (16) and Rosenhan and London (20) have shown that unhypnotizable individuals may increase their performance on motor tasks in response to hypnotic-induction procedures more than hypnotizable individuals. One must be careful not to draw the erroneous conclusion that, therefore, the unhypnotizable group had in fact been hypnotized since they were still unable to respond to hypnotic suggestions. They merely again documented that behavioral compliance is not the same as being hypnotized. In fact, these studies are somewhat difficult to interpret. There may well be an important interaction between subjects' initial failure to respond to hypnosis and a compensatory eagerness to do well on tasks that they are able to carry out -- those that do not involve the hypnotic phenomenon, confounded by complex order effects (see ref. 7). Indeed, it is because of these concerns that the McGlashan et al. (17) study sought to convince the unhypnotizable individuals that they were able to respond to hypnosis. This manipulation was intended to help make the response of the unhypnotizable subjects to the hypnotic procedure more closely analogous to their response to placebo. We would like to generalize findings with this group to the effect of hypnotic induction procedures on unhypnotizable individuals in a clinical context -- patients who lack the skill of entering hypnosis but do not perceive themselves as unresponsive. Under such circumstances, the hypnotic procedure appears to us as far from inert even with subjects who do not readily show evidence of distorted perception or memory in response to suggestions.
167 HYPNOTIC CONTROL OF PAIN
EFFECTS OF HYPNOTIC INDUCTION IN THE CLINICAL CONTEXT
The use of a hypnotic procedure alters many aspects of the doctor-patient relationship. Furthermore, by asking the patient to attend to some ideas and to ignore others, important cognitive changes may be brought about. Not only can the hypnotic induction procedure affect the patient directly, but it may also radically change the way the physician behaves, which, in turn, can have profound effects on what the patient experiences.
Consider some examples. Few individuals find it easy to sit still for 30 or 40 min without fidgeting or moving about, yet an overhwelming majority of individuals will remain virtually motionless during a lengthy induction procedure, regardless of their response. Somehow, most induction procedures successfully capture the patient's attention sufficiently to inhibit much extraneous movement. Though these procedures will not have the effect of inducing hypnosis with subjects lacking the ability to respond, such subjects will, nonetheless, tend to lose track of time and may feel that they have been affected in some undefinable fashion. These are effects which may be impressive to the patient and have clinical consequences, but which should be recognized as related to the procedure of hypnotic induction rather than following from the patient's actually entering hypnosis.
For example, few patients will happily sit through a lengthy harangue on the evils of smoking from their physician, yet virtually all patients seeking help for smoking cessation, exposed to a brief hypnotic-induction procedure, given relaxation instructions, and told to close their eyes, will quietly sit through a lengthy harangue without fidgeting or any other behavioral signs of discomfort. Typically, they will attend to such a lecture with far more care than usual even though they show no evidence of being able to respond positively to any hypnotic suggestion. Indeed, a fair number of unhypnotized subjects will even stop smoking following such a procedure.
Consider the effect of hypnosis in the dental procedure with an anxious patient. Instead of minimizing the patient's fears and treating them with annoyance, the dentist deciding to use hypnosis will show concern about the patient and his comfort, establish rapport, and then carefully induce hypnosis, even though this might not otherwise be representative of his normal chairside behavior. Throughout the hypnotic session he will maintain an almost continuous stream of suggestions and remain very sensitive to the patient's reactions. While he may have given suggestions of analgesia, the dentist schooled in the use of hypnosis will promptly terminate any activity that brings about even minor evidence of discomfort, renewing his suggestions of relaxation, and proceeding subsequently only with great caution, often augmenting hypnotic analgesia with a suitable amount of xylocaine.
From the patient's point of view, even if he is not hypnotizable, the hypnotic situation is radically different from his usual dental encounter. Instead of feeling that the dentist wants to get on with the technical aspects of repairing his
168 HYPNOTIC CONTROL OF PAIN
teeth, the dentist seems more concerned with his comfort during the procedure. Instead of being largely ignored, with the dentist either quietly doing his work or maintaining a conversation with his nurse, there is a continuous show of interest on the part of the dentist and an obvious sensitivity to even slight evidence of discomfort. It is hardly surprising that under such circumstances patients become more relaxed, trusting, and show an increased ability to tolerate discomfort. These effects need have little to do with hypnosis; rather they may be a function of the patient's increased feeling of control and safety.
Several studies have shown that giving subjects control of when painful stimuli are administered (1), or the belief that they could control the stimuli (4,23), or even only the belief that they could terminate stimuli (19), would increase the tolerance for discomfort and decrease their physiological responses to stimuli. Analogously, it is well known that procedures which give patients the feeling of control in a dental context can, in and of themselves, bring about a marked rise in pain threshold. Similarly, the patient comes to believe that the dentist will not inflict serious pain, another factor that increases pain tolerance since a small amount of pain no longer serves to signal the inevitable advent of more severe pain. The reduction of anxiety which follows from the total procedure also serves to decrease the sensitivity to pain. Simply being talked through a dental procedure is infinitely more reassuring than being left to one's own devices, which permits fears and fantasies to multiply. Note that both the direct and indirect effects discussed above, which follow from the use of hypnotic procedures, have little to do with the patient's entering hypnosis. Nonetheless, they profoundly alter his experience. This may well account for the fact that dentists report 80 to 90% success with the use of hypnosis as an analgesia, while only 15 to 20% of patients are able to achieve a moderately profound hypnotic response which would lead to dental analgesia in the sense of a hypnotically suggested negative hallucination for pain.
Hypnosis in the Treatment of Cancer
Though only 38 to 60% 6 of patients with terminal cancer suffer sever pain, the profound and progressive sense of isolation, the abandonment of hope, the feeling of helplessness in the face of this disease, and the increasing loneliness as family and friends, as well as caretakers, gradually withdraw, serve to focus the patient on his body and accentuate the severity of his pain. In turn, the pain serves to prevent the patient from enjoying some of the few pleasures that remain, and at times the pain itself and behavior related to pain become the principal means of communicating with the outside world.
I have had the opportunity of treating a number of patients with terminal cancer, and certainly those who are fortunate enough to have the skill of entering profound hypnosis can derive a remarkable degree of relief. However, I have
169 HYPNOTIC CONTROL OF PAIN
become increasingly aware of the complex and important role that the hypnotic-induction procedure and its consequences not related to the presence of hypnosis, may serve in reversing what had appeared to be a progressive worsening of the patient's overall condition. Thus, the induction of hypnosis and training in self-hypnosis provide the opportunity for someone to offer relief in a manner that involves the patient's active participation. In the context of a structured treatment program, those around the patient can be assigned responsibility to help him to better achieve the skill of pain control. For the first time in the course of the disease it becomes possible for the patient to succeed in accomplishing something of importance to himself and to focus on one or another aspect of improvement, be it increased pain tolerance, the decrease of nausea, a modest gain in weight, or the ability to read or dictate correspondence; the specifics of the accomplishment matter little, the fact that progress can he perceived matters a great deal. Some modest sign of progress is important not only for the patient, but at times, even more so to help those around him to maintain their ability to interact meaningfully, to focus on the positive things that can be shared rather than the pain and suffering that may be as unbearable to those close to the patient as they are to him.
Much has been written about the importance of factors such as these in making what remains of life livable and meaningful, but it has rarely been emphasized how the use of the hypnotic situation can provide some of the contexts which, for many patients, permit the kind of changes I have tried to sketch above. While the patient who is able to enter hypnosis will have the benefits of suggested analgesia as well as the benefits that follow from the induction procedure, many of the changes that hypnotic techniques, particularly the use of self-hypnosis, can bring about in the patient's perception of the situation and in his interaction with those around him have little or nothing to do with his ability to enter hypnosis. On the contrary, they reflect the response on the part, of the physician, who suddenly feels there is something that can be offered to the patient to give him relief, on the part of the family, who suddenly may be encouraged to share positive experiences with the patient and find the interaction less enervating, and on the part of the patient, who begins again to feel able to control some aspects of his experience.
Cognitive Changes Associated with Hypnotic Induction
An effort has been made to separate the effects of hypnosis, which depend upon the individual's ability to be hypnotized from other effects that are commonly seen as a consequence of a hypnotic induction procedure but which can be identified, separated, and studied in their own right. Individuals with moderate pain, agreeing to be hypnotized, will typically relax in response to appropriate suggestions even though they may not be hypnotizable. Not only do they relax but, as they do, there is the implicit demand that they suppress pain-related behavior. There is a very strong tendency for individuals not only
170 HYPNOTIC CONTROL OF PAIN
to suppress the outward signs of pain, but also to report subsequently that they felt more comfortable during the trance procedure. An interesting study by Lanzetta et al. (14) suggests a relevant mechanism. They reported that in trials when subjects were required to convince an observer -- by means of facial and postural expressions -- that a shock was not painful, the subjects produced smaller skin conductance responses and assigned lower ratings of shock intensity than on trials where they were not required to suppress external evidence of pain. Since the hypnotic procedure may implicitly require the suppression of pain behavior, a modest degree of relief may be anticipated simply as a function of that process itself.
We have tried to suggest that much may be learned by analyzing the effects of the induction procedure independently from the effects of hypnosis. On the one hand, this will provide a better understanding of how hypnotic procedures relieve pain. Of at least equal importance, it will help further the systematic study of psychological processes in general that affect the pain experience.
SUMMARY
Hypnotic anesthesia for major surgery documents the effectiveness of psychological means of pain control in suitable individuals. We have considered some of the mechanisms that are involved in this process. The most important factor appears to be the patient's ability to be hypnotized, a skill that is an enduring trait of the individual.
That skill appears unrelated to the placebo response and can be brought forth not only by formal trance induction procedures but also under other circumstances, only some of which have thus far been specified.
In addition to the effect of hypnosis, which require the patient to have the ability to respond, the hypnotic-induction procedure in and of itself can have profound effects, even on the unhypnotizable individual. While this includes nonspecific effects, the induction procedure also has consequences that can be identified and studied in their own right. Thus, it incorporates techniques that refocus the patient's attention and may profoundly alter other important cognitive processes. Further, the effort to induce hypnosis may alter the doctor-patient relationship and affect the behavior of both the physician and others close to the patient, leading to enduring consequences which often have salutary effects on the patient's overall comfort and ability to cope.
Much of the confusion and controversy concerning the effects of hypnosis is due to the fact that one tends to group together those effects which follow when an individual is hypnotized, that relate primarily to the individual's hypnotic ability, with those effects which stem directly and indirectly from being exposed to a hypnotic induction procedure and are unrelated to hypnotizability.
An effort has been made to distinguish conceptually between these different mechanisms that may independently affect the pain experience. While there is a specific effect of hypnosis on pain, related primarily to the patient's ability
171 HYPNOTIC CONTROL OF PAIN
to enter hypnosis, the sum total of other mechanisms, which alter expectancies and can bring about other cognitive changes in both the patient and those around him, may in many instances be equally important. An understanding of these separate aspects and an analysis of the mechanisms involved will not only lead to a better understanding of the variety of processes that occur under the heading of hypnotically induced analgesia, but also provide much needed links between apparently disparate studies designed to explore the role of psychological factors on the pain experience. One would hope that such an approach will make the hypnotic control of pain available to all those individuals who are fortunate to have the prerequisite ability to enter hypnosis, while at the same time it should help to develop the other psychological procedures which can effectively modulate the pain experience and thereby minimize unnecessary suffering.
ACKNOWLEDGMENTS
The substantive research upon which this chapter is based was supported in part by Grant No. MH-9156 from the National Institute of Mental Health. I would like to express my appreciation to my colleagues, David R. Dinges, Frederick J. Evans, Emily Carota Orne, William M. Waid, and Stuart K. Wilson for their helpful comments in the preparation of this chapter.
REFERENCES
1. Averill, J. R. (1973): Personal control over aversive stimuli and its relationship to stress. Psychol. Bull., 80:286-303.
2. Banyai, E. I., and Hilgard, E. R. (1976): A comparison of active-alert hypnotic induction with traditional relaxation induction. J. Abnorm. Psychol., 85:218-224.
3. Barber, J. (1977): Rapid induction analgesia: A clinical report. Am. J. Clin. Hypn., 19:138-147.
4. Bowers, K. (1968): Pain, anxiety and perceived control. J. Consul. Clin. Psychol., 32:596-602.
5. Dorpat, T. L., and Holmes, T. H. (1955): Mechanisms of skeletal muscle pain and fatigue. Arch. Neurol. Psychiatr., 74:628-640.
6. Esdaile, J. (1957): Hypnosis in Medicine and Surgery. Introduction and supplementary reports by Wm. S. Kroger. Julian, New York. (Originally titled Mesmerism in India, 1850.)
7. Evans, F. J., and Orne, M. T. (1965): Motivation, performance, and hypnosis. Int. J. Clin. Exp. Hypn., 13:103-116.
8. Foley, K. M. (1979): Pain syndromes in patients with cancer. In: Advances in Pain Research and Therapy. Vol. 2. edited by J. J. Bonica and V. Ventafridda. Raven Press, New York (in press).
9. Glass, D. C., Singer, J. E., Leonard, H. S., Krants, D., Cohen, S., and Cummings, H. (1973); Perceived control of aversive stimulation and the reduction of stress responses. J. Pers., 41:577595.
10. Gottfredson, D. K. (1973): Hypnosis as an anesthetic in dentistry. Doctoral dissertation, Department of Psychology, Brigham Young University. Dissertation Abstr. Int., 33:7-B.
11. Hilgard, E. R. (1965): Hypnotic Susceptibility. Harcourt, Brace & World, New York.
12. Hilgard, E. R., and Hilgard, J. R. (1975): Hypnosis in the Relief of Pain. Kaufman, Los Altos, California.
13. Hilgard, E. R., and Morgan, A. H. (1975): Heart rate and blood pressure in the study of laboratory pain in man under normal conditions and as influenced by hypnosis. Acta Neurobiol. Exp., 35:741-759.
172 HYPNOTIC CONTROL OF PAIN
14. Lanzetta, J., Cartwright-Smith, J., and Kleck, R. E. Effects of nonverbal
dissimulation on emotional experiencing and automatic arousal. J. Pers. Soc.
Pychol. 33:354-370.
15. Lasagna, L.. Tetreault, L., and Fallis, N. E. Analgesic drugs and experimental ischemic pain. Fed. Proc., 21:326.
16. London, P., and Fuhrer, M. (1961): Hypnosis, motivation, and performance. J. Pers., 29:321-333.
17. McGlashan, T. H., Evans, F. J., and Orne, M. T. The nature of hypnotic analgesia and placebo response to experimental pain. Psychosom. Med.. 31:227-246.
18. Orne, M. T. (1976): Mechanisms of hypnotic pain control. In: Advances in Pain Research and Therapy. Vol. 1, edited by J. J. Bonica and D-Albe-Fessard, pp. 717-726. Raven Press, New York.
19. Orne, M. T. (1977): The construct of hypnosis: Implications of the definition for research and practice: Ann. N. Y. Acad. Sci., 296:14-33.
20. Rosenhan, D., and London, P. Hypnosis: Expectation, susceptibility, and performance. J. Abnorm. Soc. Psychol, 66:77-81.
21. Sarbin, T. R. (1956): Physiological effects of hypnotic stimulation. In: Hypnosis and its Therapeutic Applications, edited by R. M. Dorcus, pp. 41-57. McGraw-Hill, New York.
22. Shor, R. E., and Orne, E. C. (1962): Harvard Group Scale of Hypnotic Susceptibility: Form A. Consulting Psychologists Press, Palo Alto, California.
23. Staub, E., Tursky, B., and Schwartz, G. E. (1979): Self-control and predictability: Their effects on reactions to aversive stimulation. J. Pers. Soc. Psychol., 18:157-162.
24. Sternbach, R. A. (1968): Pain: A Psychophysiological Analysis. Academic Press, New York.
25. Weitzenhoffer, A. M., and Hilgard, E. R.: Stanford Hypnotic Susceptibility Scale, Forms A and B. Consulting Psychologists Press, Palo Alto, California.
26. Weitzenhoffer, A. M., and Hilgard, E. R. (1962): Stanford Hypnotic Susceptibility Scale, Form C. Consulting Psychologists Press, Palo Alto, California.
Figure 1 (p. 162) (from Hilgard, E.R., & Morgan, A.H. Heart rate and blood pressure in the study of laboratory pain in man under normal conditions and as influenced by hypnosis. Acta Neurobiologiae Experimentalis, 1975, 35, 741-759.) is reproduced here with the kind permission of the editor of the Acta Neurobiologiae Experimentalis.
Figure 2 (p. 165) (from McGlashan, T.H., Evans, F.J., & Orne, M.T. The nature of hypnotic analgesia and placebo response to experimental pain. Psychosomatic Medicine, 1969, 32, 227-246) ©1969 by American Psychosomatic Society, Inc., is reproduced here with the kind permission of Lippincott Williams & Wilkins ©.